Design of biodegradable, implantable devices towards clinical translation
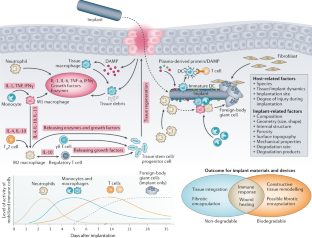
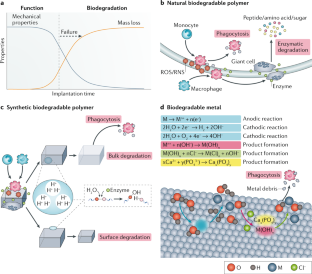
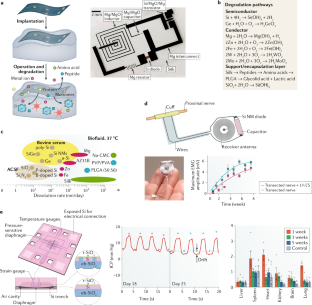
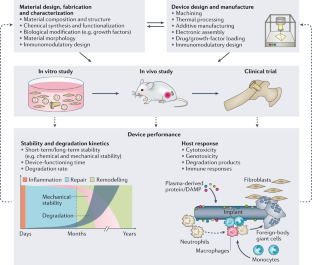
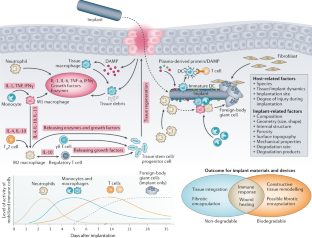
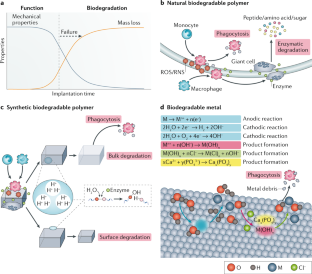
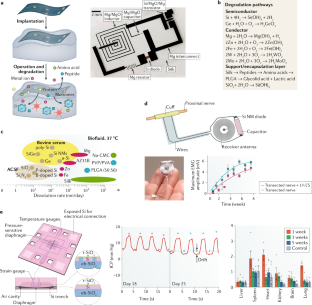
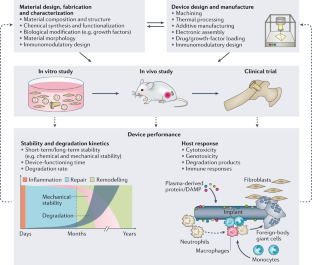
Biodegradable materials, including natural and synthetic polymers and hydrolyzable metals, constitute the main components of temporary, implantable medical devices. Besides the intrinsic properties of the materials, the most critical factor determining the successful clinical outcome of implantable and degradable devices is the host response, particularly the immune response, which largely depends on the material features and degradation mechanisms. In this Review, we first survey the state of the art in terms of materials options for use in biodegradable medical devices, focusing on degradation mechanisms and their control. In particular, we highlight silk, which is emerging as an important polymer, owing to its mechanical robustness, bioactive component sequestration, degradability without problematic metabolic products and biocompatibility. We then discuss the host response to these biodegradable materials in terms of dynamic tissue–implant interfaces. Next, we examine the clinical translation of three leading biodegradable material systems — natural and synthetic biodegradable polymers and biodegradable metals — and the related challenges in the context of orthopaedic fixation devices, cardiovascular stents and biodegradable electronic devices. Looking to the future, we propose updated material design strategies to improve the clinical outcomes for these biodegradable medical devices.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
133,45 € per year
only 11,12 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others

Self-healing polyurethane-elastomer with mechanical tunability for multiple biomedical applications in vivo
Article Open access 20 July 2021

Bioactive potential of natural biomaterials: identification, retention and assessment of biological properties
Article Open access 19 March 2021

Nitric oxide-generating metallic wires for enhanced metal implants
Article Open access 17 July 2024
References
- Kurtz, S., Ong, K., Lau, E., Mowat, F. & Halpern, M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J. Bone Joint Surg. Am.89, 780–785 (2007). Google Scholar
- Cobelli, N., Scharf, B., Crisi, G. M., Hardin, J. & Santambrogio, L. Mediators of the inflammatory response to joint replacement devices. Nat. Rev. Rheumatol.7, 600–608 (2011). CASGoogle Scholar
- Hubbell, J. A. & Langer, R. Translating materials design to the clinic. Nat. Mater.12, 963–966 (2013). CASGoogle Scholar
- Farra, R. et al. First-in-human testing of a wirelessly controlled drug delivery microchip. Sci. Transl Med.4, 122ra121 (2012). Google Scholar
- Nichols, S. P., Koh, A., Storm, W. L., Shin, J. H. & Schoenfisch, M. H. Biocompatible materials for continuous glucose monitoring devices. Chem. Rev.113, 2528–2549 (2013). CASGoogle Scholar
- Rosen, M. R., Robinson, R. B., Brink, P. R. & Cohen, I. S. The road to biological pacing. Nat. Rev. Cardiol.8, 656–666 (2011). Google Scholar
- Wykrzykowska, J. J. et al. Bioresorbable scaffolds versus metallic stents in routine PCI. N. Engl. J. Med.376, 2319–2328 (2017). CASGoogle Scholar
- Devi, K. S. & Vasudevan, P. Absorbable surgical sutures. J. Macromol. Sci. C25, 315–324 (1985). Google Scholar
- Hjort, H., Mathisen, T., Alves, A., Clermont, G. & Boutrand, J. P. Three-year results from a preclinical implantation study of a long-term resorbable surgical mesh with time-dependent mechanical characteristics. Hernia16, 191–197 (2012). CASGoogle Scholar
- Serruys, P. W. et al. A bioabsorbable everolimus-eluting coronary stent system (ABSORB): 2-year outcomes and results from multiple imaging methods. Lancet373, 897–910 (2009). CASGoogle Scholar
- Cassese, S. et al. Everolimus-eluting bioresorbable vascular scaffolds versus everolimus-eluting metallic stents: a meta-analysis of randomised controlled trials. Lancet387, 537–544 (2016). CASGoogle Scholar
- Cha, G. D., Kang, D., Lee, J. & Kim, D. H. Bioresorbable electronic implants: history, materials, fabrication, devices, and clinical applications. Adv. Healthc. Mater.8, e1801660 (2019). Google Scholar
- Liu, Y., Zheng, Y. & Hayes, B. Degradable, absorbable or resorbable — what is the best grammatical modifier for an implant that is eventually absorbed by the body? Sci. China Mater.60, 377–391 (2017). CASGoogle Scholar
- Anderson, J. M., Rodriguez, A. & Chang, D. T. Foreign body reaction to biomaterials. Semin. Immunol.20, 86–100 (2008). CASGoogle Scholar
- Chandorkar, Y., Ravikumar, K. & Basu, B. The foreign body response demystified. ACS Biomater. Sci. Eng.5, 19–44 (2019). Google Scholar
- Kumar, V., Abbas, A. K., & Aster, J. C. Robbins & Cotran Pathologic Basis of Disease 9th edn (Elsevier/Saunders, 2015).
- Julier, Z., Park, A. J., Briquez, P. S. & Martino, M. M. Promoting tissue regeneration by modulating the immune system. Acta Biomater.53, 13–28 (2017). CASGoogle Scholar
- Woodruff, M. A. & Hutmacher, D. W. The return of a forgotten polymer — polycaprolactone in the 21st century. Prog. Polym. Sci.35, 1217–1256 (2010). CASGoogle Scholar
- Iwasaki, A. & Medzhitov, R. Regulation of adaptive immunity by the innate immune system. Science327, 291–295 (2010). CASGoogle Scholar
- Franz, S., Rammelt, S., Scharnweber, D. & Simon, J. C. Immune responses to implants – a review of the implications for the design of immunomodulatory biomaterials. Biomaterials32, 6692–6709 (2011). CASGoogle Scholar
- Nilsson, B., Korsgren, O., Lambris, J. D. & Ekdahl, K. N. Can cells and biomaterials in therapeutic medicine be shielded from innate immune recognition? Trends Immunol.31, 32–38 (2010). CASGoogle Scholar
- Mantovani, A., Biswas, S. K., Galdiero, M. R., Sica, A. & Locati, M. Macrophage plasticity and polarization in tissue repair and remodelling. J. Pathol.229, 176–185 (2013). CASGoogle Scholar
- Sica, A. & Mantovani, A. Macrophage plasticity and polarization: in vivo veritas. J. Clin. Invest.122, 787–795 (2012). CASGoogle Scholar
- Mantovani, A. et al. The chemokine system in diverse forms of macrophage activation and polarization. Trends Immunol.25, 677–686 (2004). CASGoogle Scholar
- Wynn, T. A. & Vannella, K. M. Macrophages in tissue repair, regeneration, and fibrosis. Immunity44, 450–462 (2016). CASGoogle Scholar
- Wynn, T. A. & Barron, L. Macrophages: master regulators of inflammation and fibrosis. Semin. Liver Dis.30, 245–257 (2010). CASGoogle Scholar
- Willenborg, S. et al. CCR2 recruits an inflammatory macrophage subpopulation critical for angiogenesis in tissue repair. Blood120, 613–625 (2012). CASGoogle Scholar
- Murray, P. J. & Wynn, T. A. Protective and pathogenic functions of macrophage subsets. Nat. Rev. Immunol.11, 723–737 (2011). CASGoogle Scholar
- Shouval, D. S. et al. Interleukin-10 receptor signaling in innate immune cells regulates mucosal immune tolerance and anti-inflammatory macrophage function. Immunity40, 706–719 (2014). CASGoogle Scholar
- Zigmond, E. et al. Macrophage-restricted interleukin-10 receptor deficiency, but not IL-10 deficiency, causes severe spontaneous colitis. Immunity40, 720–733 (2014). CASGoogle Scholar
- Raimondo, T. M. & Mooney, D. J. Functional muscle recovery with nanoparticle-directed M2 macrophage polarization in mice. Proc. Natl Acad. Sci. USA115, 10648–10653 (2018). CASGoogle Scholar
- Brown, B. N., Sicari, B. M. & Badylak, S. F. Rethinking regenerative medicine: a macrophage-centered approach. Front. Immunol.5, 510 (2014). Google Scholar
- Agrawal, V. et al. Epimorphic regeneration approach to tissue replacement in adult mammals. Proc. Natl Acad. Sci. USA107, 3351–3355 (2010). CASGoogle Scholar
- Biswas, S. K. & Mantovani, A. Macrophage plasticity and interaction with lymphocyte subsets: cancer as a paradigm. Nat. Immunol.11, 889–896 (2010). CASGoogle Scholar
- Scarritt, M. E., Londono, R. & Badylak, S. F. in The Immune Response to Implanted Materials and Devices: The Impact of the Immune System on the Success of an Implant (ed. Corradetti, B.) 1–14 (Springer, 2017).
- Sadtler, K. et al. Developing a pro-regenerative biomaterial scaffold microenvironment requires T helper 2 cells. Science352, 366–370 (2016). CASGoogle Scholar
- Feiner, R. & Dvir, T. Tissue–electronics interfaces: from implantable devices to engineered tissues. Nat. Rev. Mater.3, 17076 (2017). Google Scholar
- Moshayedi, P. et al. The relationship between glial cell mechanosensitivity and foreign body reactions in the central nervous system. Biomaterials35, 3919–3925 (2014). CASGoogle Scholar
- Nguyen, J. K. et al. Mechanically-compliant intracortical implants reduce the neuroinflammatory response. J. Neural. Eng.11, 056014 (2014). Google Scholar
- Rivnay, J., Wang, H., Fenno, L., Deisseroth, K. & Malliaras, G. G. Next-generation probes, particles, and proteins for neural interfacing. Science Adv.3, e1601649 (2017). Google Scholar
- Subbaroyan, J., Martin, D. C. & Kipke, D. R. A finite-element model of the mechanical effects of implantable microelectrodes in the cerebral cortex. J. Neural Eng.2, 103–113 (2005). Google Scholar
- Veiseh, O. et al. Size- and shape-dependent foreign body immune response to materials implanted in rodents and non-human primates. Nat. Mater.14, 643–651 (2015). CASGoogle Scholar
- Sanders, J. E., Stiles, C. E. & Hayes, C. L. Tissue response to single-polymer fibers of varying diameters: evaluation of fibrous encapsulation and macrophage density. J. Biomed. Mater. Res.52, 231–237 (2000). CASGoogle Scholar
- Matlaga, B. F., Yasenchak, L. P. & Salthouse, T. N. Tissue response to implanted polymers: the significance of sample shape. J. Biomed. Mater. Res.10, 391–397 (1976). CASGoogle Scholar
- Salthouse, T. N. Some aspects of macrophage behavior at the implant interface. J. Biomed. Mater. Res.18, 395–401 (1984). CASGoogle Scholar
- Madden, L. R. et al. Proangiogenic scaffolds as functional templates for cardiac tissue engineering. Proc. Natl Acad. Sci.USA107, 15211–15216 (2010). CASGoogle Scholar
- Sussman, E. M., Halpin, M. C., Muster, J., Moon, R. T. & Ratner, B. D. Porous implants modulate healing and induce shifts in local macrophage polarization in the foreign body reaction. Ann. Biomed. Eng.42, 1508–1516 (2014). Google Scholar
- Young, J. L. et al. In vivo response to dynamic hyaluronic acid hydrogels. Acta Biomater.9, 7151–7157 (2013). CASGoogle Scholar
- Amini, A. R., Wallace, J. S. & Nukavarapu, S. P. Short-term and long-term effects of orthopedic biodegradable implants. J. Long Term Eff. Med. Implants21, 93–122 (2011). CASGoogle Scholar
- Gallagher, W. M. et al. Molecular basis of cell–biomaterial interaction: insights gained from transcriptomic and proteomic studies. Biomaterials27, 5871–5882 (2006). CASGoogle Scholar
- Boss, J. H., Shajrawi, I., Aunullah, J. & Mendes, D. G. The relativity of biocompatibility. a critique of the concept of biocompatibility. Isr. J. Med. Sci.31, 203–209 (1995). CASGoogle Scholar
- Siebers, M. C., ter Brugge, P. J., Walboomers, X. F. & Jansen, J. A. Integrins as linker proteins between osteoblasts and bone replacing materials. A critical review. Biomaterials26, 137–146 (2005). CASGoogle Scholar
- Nuss, K. M. & von Rechenberg, B. Biocompatibility issues with modern implants in bone - a review for clinical orthopedics. Open Orthop. J.2, 66–78 (2008). Google Scholar
- Ekdahl, K. N. et al. Innate immunity activation on biomaterial surfaces: a mechanistic model and coping strategies. Adv. Drug Del. Rev.63, 1042–1050 (2011). CASGoogle Scholar
- Xu, L.-C., Bauer, J. W. & Siedlecki, C. A. Proteins, platelets, and blood coagulation at biomaterial interfaces. Colloids Surf. B Biointerfaces124, 49–68 (2014). CASGoogle Scholar
- Engberg, A. E. et al. Blood protein-polymer adsorption: implications for understanding complement-mediated hemoincompatibility. J. Biomed. Mater. Res. A97A, 74–84 (2011). CASGoogle Scholar
- Ferraz, N., Ott, M. K. & Hong, J. Time sequence of blood activation by nanoporous alumina: studies on platelets and complement system. Microsc. Res. Tech.73, 1101–1109 (2010). CASGoogle Scholar
- Willumeit-Römer, R. The interface between degradable Mg and tissue. JOM71, 1447–1455 (2019). Google Scholar
- Lee, J.-W. et al. Long-term clinical study and multiscale analysis of in vivo biodegradation mechanism of Mg alloy. Proc. Natl Acad. Sci. USA113, 716–721 (2016). CASGoogle Scholar
- Kenawy, H. I., Boral, I. & Bevington, A. Complement-coagulation cross-talk: a potential mediator of the physiological activation of complement by low pH. Front. Immunol.6, 215 (2015). Google Scholar
- Yang, H. et al. Evolution of the degradation mechanism of pure zinc stent in the one-year study of rabbit abdominal aorta model. Biomaterials145, 92–105 (2017). CASGoogle Scholar
- Holland, C., Numata, K., Rnjak-Kovacina, J. & Seib, F. P. The biomedical use of silk: past, present, future. Adv. Healthc. Mater.8, 1800465 (2019). Google Scholar
- Huang, W., Ling, S., Li, C., Omenetto, F. G. & Kaplan, D. L. Silkworm silk-based materials and devices generated using bio-nanotechnology. Chem. Soc. Rev.47, 6486–6504 (2018). CASGoogle Scholar
- Zhou, Z. et al. Engineering the future of silk materials through advanced manufacturing. Adv. Mater.30, 1706983 (2018). Google Scholar
- Keane, T. J., Swinehart, I. T. & Badylak, S. F. Methods of tissue decellularization used for preparation of biologic scaffolds and in vivo relevance. Methods84, 25–34 (2015). CASGoogle Scholar
- Brown, B. N. & Badylak, S. F. in Translating Regenerative Medicine to the Clinic (ed. Laurence, J.) 11–29 (Academic, 2016).
- Huleihel, L. et al. Matrix-bound nanovesicles within ECM bioscaffolds. Science Adv.2, e1600502 (2016). Google Scholar
- Christman, K. L. Biomaterials for tissue repair. Science363, 340–341 (2019). CASGoogle Scholar
- Prestwich, G. D. & Atzet, S. in Biomaterials Science 3rd edn (eds Ratner, B. D., Hoffman, A. S., Schoen, F. J. & Lemons, J. E.) 195–209 (Academic, 2013).
- Schmitt, E. E. & Polistina, R. A. Surgical sutures. US patent US3297033A (1967).
- Schmitt, E. E., Epstein, M. & Polistina, R. A. Process for polymerizing a glycolide. US patent US3442871A (1969).
- Schmitt, E. E. & Polistina, R. A. Polyglycolic acid prosthetic devices. US patent US3463158A (1969).
- Middleton, J. C. & Tipton, A. J. Synthetic biodegradable polymers as orthopedic devices. Biomaterials21, 2335–2346 (2000). CASGoogle Scholar
- Nair, L. S. & Laurencin, C. T. Biodegradable polymers as biomaterials. Prog. Polym. Sci.32, 762–798 (2007). CASGoogle Scholar
- Vroman, I. & Tighzert, L. Biodegradable polymers. Materials2, 307–344 (2009). CASGoogle Scholar
- Tian, H., Tang, Z., Zhuang, X., Chen, X. & Jing, X. Biodegradable synthetic polymers: preparation, functionalization and biomedical application. Prog. Polym. Sci.37, 237–280 (2012). CASGoogle Scholar
- McMahon, S. et al. Bio-resorbable polymer stents: a review of material progress and prospects. Prog. Polym. Sci.83, 79–96 (2018). CASGoogle Scholar
- Regazzoli, D., Leone, P. P., Colombo, A. & Latib, A. New generation bioresorbable scaffold technologies: an update on novel devices and clinical results. J. Thorac. Dis.9, S979–S985 (2017). Google Scholar
- Ulery, B. D., Nair, L. S. & Laurencin, C. T. Biomedical applications of biodegradable polymers. J. Polym. Sci. B Polym. Phys.49, 832–864 (2011). CASGoogle Scholar
- Hermawan, H. Updates on the research and development of absorbable metals for biomedical applications. Prog. Biomater.7, 93–110 (2018). CASGoogle Scholar
- Venezuela, J. & Dargusch, M. S. The influence of alloying and fabrication techniques on the mechanical properties, biodegradability and biocompatibility of zinc: a comprehensive review. Acta Biomater.87, 1–40 (2019). CASGoogle Scholar
- Han, H.-S. et al. Current status and outlook on the clinical translation of biodegradable metals. Mater. Today23, 57–71 (2019). CASGoogle Scholar
- Bowen, P. K., Drelich, J. & Goldman, J. Zinc exhibits ideal physiological corrosion behavior for bioabsorbable stents. Adv. Mater.25, 2577–2582 (2013). CASGoogle Scholar
- Mostaed, E., Sikora-Jasinska, M., Drelich, J. W. & Vedani, M. Zinc-based alloys for degradable vascular stent applications. Acta Biomater.71, 1–23 (2018). CASGoogle Scholar
- Haude, M. et al. Safety and performance of the second-generation drug-eluting absorbable metal scaffold in patients with de-novo coronary artery lesions (BIOSOLVE-II): 6 month results of a prospective, multicentre, non-randomised, first-in-man trial. Lancet387, 31–39 (2016). CASGoogle Scholar
- Yin, L. et al. Dissolvable metals for transient electronics. Adv. Funct. Mater.24, 645–658 (2014). CASGoogle Scholar
- Laskin, D. L., Sunil, V. R., Gardner, C. R. & Laskin, J. D. Macrophages and tissue injury: agents of defense or destruction? Annu. Rev. Pharmacol. Toxicol.51, 267–288 (2011). CASGoogle Scholar
- Xia, Z. & Triffitt, J. A review on macrophage responses to biomaterials. Biomed. Mater.1, R1–R9 (2006). CASGoogle Scholar
- Horan, R. L. et al. In vitro degradation of silk fibroin. Biomaterials26, 3385–3393 (2005). CASGoogle Scholar
- Brown, J., Lu, C. L., Coburn, J. & Kaplan, D. L. Impact of silk biomaterial structure on proteolysis. Acta Biomater.11, 212–221 (2015). CASGoogle Scholar
- Wang, Y. et al. In vivo degradation of three-dimensional silk fibroin scaffolds. Biomaterials29, 3415–3428 (2008). CASGoogle Scholar
- Brown, B., Lindberg, K., Reing, J., Stolz, D. B. & Badylak, S. F. The basement membrane component of biologic scaffolds derived from extracellular matrix. Tissue Eng.12, 519–526 (2006). CASGoogle Scholar
- Bonnans, C., Chou, J. & Werb, Z. Remodelling the extracellular matrix in development and disease. Nat. Rev. Mol. Cell Biol.15, 786–801 (2014). CASGoogle Scholar
- Lu, P., Takai, K., Weaver, V. M. & Werb, Z. Extracellular matrix degradation and remodeling in development and disease. Cold Spring Harb. Perspect. Biol.3, a005058 (2011). Google Scholar
- Gilbert, T. W., Stewart-Akers, A. M. & Badylak, S. F. A quantitative method for evaluating the degradation of biologic scaffold materials. Biomaterials28, 147–150 (2007). CASGoogle Scholar
- Valentin, J. E., Stewart-Akers, A. M., Gilbert, T. W. & Badylak, S. F. Macrophage participation in the degradation and remodeling of extracellular matrix scaffolds. Tissue Eng. Part A15, 1687–1694 (2009). CASGoogle Scholar
- Carey, L. E. et al. In vivo degradation of 14C-labeled porcine dermis biologic scaffold. Biomaterials35, 8297–8304 (2014). CASGoogle Scholar
- Azevedo, H. S. & Reis, R. L. in Biodegradable Systems in Tissue Engineering and Regenerative Medicine Ch. 12 (eds Reis, R. L. & Román, J. S.) (CRC, 2004).
- Xie, F. et al. Degradation and stabilization of polyurethane elastomers. Prog. Polym. Sci.90, 211–268 (2019). CASGoogle Scholar
- Burkersroda, Fv, Schedl, L. & Göpferich, A. Why degradable polymers undergo surface erosion or bulk erosion. Biomaterials23, 4221–4231 (2002). Google Scholar
- Shasteen, C. & Choy, Y. B. Controlling degradation rate of poly(lactic acid) for its biomedical applications. Biomed. Eng. Lett.1, 163–167 (2011). Google Scholar
- Jin, L., Wu, J., Yuan, G. & Chen, T. In vitro study of the inflammatory cells response to biodegradable Mg-based alloy extract. PLOS ONE13, e0193276 (2018). Google Scholar
- Agarwal, S., Curtin, J., Duffy, B. & Jaiswal, S. Biodegradable magnesium alloys for orthopaedic applications: a review on corrosion, biocompatibility and surface modifications. Mater. Sci. Eng. C68, 948–963 (2016). CASGoogle Scholar
- Shuai, C. et al. Biodegradable metallic bone implants. Mater. Chem. Front.3, 544–562 (2019). CASGoogle Scholar
- Zheng, Y. F., Gu, X. N. & Witte, F. Biodegradable metals. Mater. Sci. Eng. R Rep.77, 1–34 (2014). Google Scholar
- Zhang, J. et al. Macrophage phagocytosis of biomedical Mg alloy degradation products prepared by electrochemical method. Mater. Sci. Eng. C75, 1178–1183 (2017). CASGoogle Scholar
- Sanchez, A. H. M., Luthringer, B. J. C., Feyerabend, F. & Willumeit, R. Mg and Mg alloys: how comparable are in vitro and in vivo corrosion rates? A review. Acta Biomater.13, 16–31 (2015). CASGoogle Scholar
- Johnston, S., Dargusch, M. & Atrens, A. Building towards a standardised approach to biocorrosion studies: a review of factors influencing Mg corrosion in vitro pertinent to in vivo corrosion. Sci. China Mater.61, 475–500 (2018). CASGoogle Scholar
- Meinel, L. et al. The inflammatory responses to silk films in vitro and in vivo. Biomaterials26, 147–155 (2005). CASGoogle Scholar
- Gross, J. E. et al. An evaluation of SERI surgical scaffold for soft-tissue support and repair in an ovine model of two-stage breast reconstruction. Plast. Reconstr. Surg.134, 700e–704e (2014). CASGoogle Scholar
- Perrone, G. S. et al. The use of silk-based devices for fracture fixation. Nat. Commun.5, 3385 (2014). Google Scholar
- Zhou, J. et al. In vitro and in vivo degradation behavior of aqueous-derived electrospun silk fibroin scaffolds. Polym. Degrad. Stab.95, 1679–1685 (2010). CASGoogle Scholar
- Altman, G. H., Horan, R. L., Collette, A. L., Chen, J. S. & Vanepps, D. Silk fibroin hydrogels and uses thereof. US patent 2011/0008406 A1 (2011).
- Jewell, M., Daunch, W., Bengtson, B. & Mortarino, E. The development of SERI ® surgical scaffold, an engineered biological scaffold. Ann. NY Acad. Sci.1358, 44–55 (2015). CASGoogle Scholar
- Thurber, A. E., Omenetto, F. G. & Kaplan, D. L. In vivo bioresponses to silk proteins. Biomaterials71, 145–157 (2015). CASGoogle Scholar
- Tsubouchi, K., Nakao, H., Igarashi, Y., Takasu, Y. & Yamada, H. Bombyx mori fibroin enhanced the proliferation of cultured human skin fibroblasts. J. Insect Biotechnol. Sericol.72, 65–69 (2003). CASGoogle Scholar
- Wray, L. S. et al. Effect of processing on silk-based biomaterials: Reproducibility and biocompatibility. J. Biomed. Mater. Res. B Appl. Biomater.99B, 89–101 (2011). CASGoogle Scholar
- Numata, K., Cebe, P. & Kaplan, D. L. Mechanism of enzymatic degradation of beta-sheet crystals. Biomaterials31, 2926–2933 (2010). CASGoogle Scholar
- Lundmark, K., Westermark, G. T., Olsén, A. & Westermark, P. Protein fibrils in nature can enhance amyloid protein A amyloidosis in mice: Cross-seeding as a disease mechanism. Proc. Natl Acad. Sci. USA102, 6098–6102 (2005). CASGoogle Scholar
- Dziki, J. et al. An acellular biologic scaffold treatment for volumetric muscle loss: results of a 13-patient cohort study. NPJ Regen. Med.1, 16008 (2016). Google Scholar
- Dziki, J. L., Sicari, B. M., Wolf, M. T., Cramer, M. C. & Badylak, S. F. Immunomodulation and mobilization of progenitor cells by extracellular matrix bioscaffolds for volumetric muscle loss treatment. Tissue Eng. Part A22, 1129–1139 (2016). CASGoogle Scholar
- Londono, R. & Badylak, S. F. Biologic scaffolds for regenerative medicine: mechanisms of in vivo remodeling. Ann. Biomed. Eng.43, 577–592 (2015). Google Scholar
- Lopresti, S. T. & Brown, B. N. in Host Response to Biomaterials: The Impact of Host Response on Biomaterial Selection (ed. Badylak, S. F.) 53–79 (Academic, 2015).
- Sicari, B. M. et al. An acellular biologic scaffold promotes skeletal muscle formation in mice and humans with volumetric muscle loss. Sci. Transl Med.6, 234ra258 (2014). Google Scholar
- Xu, H. et al. Host response to human acellular dermal matrix transplantation in a primate model of abdominal wall repair. Tissue Eng. Part A14, 2009–2019 (2008). CASGoogle Scholar
- Xu, H. et al. A porcine-derived acellular dermal scaffold that supports soft tissue regeneration: removal of terminal galactose-α-(1,3)-galactose and retention of matrix structure. Tissue Eng. Part A15, 1807–1819 (2009). CASGoogle Scholar
- Zhang, J. et al. Perfusion-decellularized skeletal muscle as a three-dimensional scaffold with a vascular network template. Biomaterials89, 114–126 (2016). CASGoogle Scholar
- Badylak, S. F., Valentin, J. E., Ravindra, A. K., McCabe, G. P. & Stewart-Akers, A. M. Macrophage phenotype as a determinant of biologic scaffold remodeling. Tissue Eng. Part A14, 1835–1842 (2008). CASGoogle Scholar
- Brown, B. N. et al. Macrophage phenotype as a predictor of constructive remodeling following the implantation of biologically derived surgical mesh materials. Acta Biomater.8, 978–987 (2012). CASGoogle Scholar
- Lloyd, C. M. & Snelgrove, R. J. Type 2 immunity: expanding our view. Sci. Immunol.3, eaat1604 (2018). Google Scholar
- Chan, A. J., Jang, J. C. & Nair, M. G. in The Th2 Type Immune Response in Health and Disease: From Host Defense and Allergy to MetabolicHomeostasisand Beyond (eds Gause, W. C. & Artis, D.) 115–130 (Springer, 2016).
- Keane, T. J., Horejs, C.-M. & Stevens, M. M. Scarring vs. functional healing: matrix-based strategies to regulate tissue repair. Adv. Drug Del. Rev.129, 407–419 (2018). CASGoogle Scholar
- Aamodt, J. M. & Grainger, D. W. Extracellular matrix-based biomaterial scaffolds and the host response. Biomaterials86, 68–82 (2016). CASGoogle Scholar
- Morris, A. H., Stamer, D. K. & Kyriakides, T. R. The host response to naturally-derived extracellular matrix biomaterials. Semin. Immunol.29, 72–91 (2017). CASGoogle Scholar
- Morris, A. H., Chang, J. & Kyriakides, T. R. Inadequate processing of decellularized dermal matrix reduces cell viability in vitro and increases apoptosis and acute inflammation in vivo. BioResearch Open Access5, 177–187 (2016). CASGoogle Scholar
- de Castro Brás, L. E., Shurey, S. & Sibbons, P. D. Evaluation of crosslinked and non-crosslinked biologic prostheses for abdominal hernia repair. Hernia16, 77–89 (2012). Google Scholar
- Jones, K. S. Effects of biomaterial-induced inflammation on fibrosis and rejection. Semin. Immunol.20, 130–136 (2008). CASGoogle Scholar
- Kim, M. S. et al. An in vivo study of the host tissue response to subcutaneous implantation of PLGA- and/or porcine small intestinal submucosa-based scaffolds. Biomaterials28, 5137–5143 (2007). CASGoogle Scholar
- Böstman, O. & Pihlajamäki, H. Clinical biocompatibility of biodegradable orthopaedic implants for internal fixation: a review. Biomaterials21, 2615–2621 (2000). Google Scholar
- Sung, H.-J., Meredith, C., Johnson, C. & Galis, Z. S. The effect of scaffold degradation rate on three-dimensional cell growth and angiogenesis. Biomaterials25, 5735–5742 (2004). CASGoogle Scholar
- Böstman, O. M. & Pihlajamäki, H. K. Adverse tissue reactions to bioabsorbable fixation devices. Clin. Orthop. Relat. Res.371, 216–227 (2000). Google Scholar
- Bergsma, J. E., de Bruijn, W. C., Rozema, F. R., Bos, R. R. M. & Boering, G. Late degradation tissue response to poly(l-lactide) bone plates and screws. Biomaterials16, 25–31 (1995). CASGoogle Scholar
- Seino, D., Fukunishi, S. & Yoshiya, S. Late foreign-body reaction to PLLA screws used for fixation of acetabular osteotomy. J. Orthop. Traumatol.8, 188–191 (2007). Google Scholar
- Jeon, H. B., Kang, D. H., Gu, J. H. & Oh, S. A. Delayed foreign body reaction caused by bioabsorbable plates used for maxillofacial fractures. Arch. Plast. Surg.43, 40–45 (2016). Google Scholar
- Gu, X., Zheng, Y., Cheng, Y., Zhong, S. & Xi, T. In vitro corrosion and biocompatibility of binary magnesium alloys. Biomaterials30, 484–498 (2009). CASGoogle Scholar
- Seitz, J.-M., Eifler, R., Bach, Fr.-W. & Maier, H. J. Magnesium degradation products: Effects on tissue and human metabolism. J. Biomed. Mater. Res. A102, 3744–3753 (2014). Google Scholar
- Xiao, C. et al. Indirectly extruded biodegradable Zn-0.05 wt% Mg alloy with improved strength and ductility: In vitro and in vivo studies. J. Mater. Sci. Technol.34, 1618–1627 (2018). Google Scholar
- Ma, J., Zhao, N., Betts, L. & Zhu, D. Bio-adaption between magnesium alloy stent and the blood vessel: a review. J. Mater. Sci. Technol.32, 815–826 (2016). Google Scholar
- Zhang, Y. et al. Implant-derived magnesium induces local neuronal production of CGRP to improve bone-fracture healing in rats. Nat. Med.22, 1160–1169 (2016). CASGoogle Scholar
- Zhao, N. & Zhu, D. Endothelial responses of magnesium and other alloying elements in magnesium-based stent materials. Metallomics7, 118–128 (2015). CASGoogle Scholar
- Kanno, T., Sukegawa, S., Furuki, Y., Nariai, Y. & Sekine, J. Overview of innovative advances in bioresorbable plate systems for oral and maxillofacial surgery. Jpn Dent. Sci. Rev.54, 127–138 (2018). Google Scholar
- Pina, S. & Ferreira, J. M. Bioresorbable plates and screws for clinical applications: a review. J. Healthc. Eng.3, 243–260 (2012). Google Scholar
- Walton, M. & Cotton, N. J. Long-term in vivo degradation of poly-L-lactide (PLLA) in bone. J. Biomater. Appl.21, 395–411 (2007). CASGoogle Scholar
- Ambrose, C. G. & Clanton, T. O. Bioabsorbable implants: review of clinical experience in orthopedic surgery. Ann. Biomed. Eng.32, 171–177 (2004). Google Scholar
- Barber, F. A., Dockery, W. D. & Hrnack, S. A. Long-term degradation of a poly-lactide co-glycolide/β-tricalcium phosphate biocomposite interference screw. Arthroscopy27, 637–643 (2011). Google Scholar
- Costi, J. J., Kelly, A. J., Hearn, T. C. & Martin, D. K. Comparison of torsional strengths of bioabsorbable screws for anterior cruciate ligament reconstruction. Am. J. Sports Med.29, 575–580 (2001). CASGoogle Scholar
- Daculsi, G., Goyenvalle, E., Cognet, R., Aguado, E. & Suokas, E. O. Osteoconductive properties of poly(96L/4D-lactide)/beta-tricalcium phosphate in long term animal model. Biomaterials32, 3166–3177 (2011). CASGoogle Scholar
- Frosch, K. H. et al. Magnetic resonance imaging analysis of the bioabsorbable Milagro™ interference screw for graft fixation in anterior cruciate ligament reconstruction. Strateg. Trauma Limb Reconstr.4, 73–79 (2009). Google Scholar
- Vonhoegen, J., John, D. & Hägermann, C. Osteoconductive resorption characteristics of a novel biocomposite suture anchor material in rotator cuff repair. J. Orthop. Surg. Res.14, 12 (2019). Google Scholar
- Aunoble, S., Clement, D., Frayssinet, P., Harmand, M. F. & Le Huec, J. C. Biological performance of a new β-TCP/PLLA composite material for applications in spine surgery: in vitro and in vivo studies. J. Biomed. Mater. Res. A78, 416–422 (2006). Google Scholar
- Chivot, M. et al. Pull-out strength of four tibial fixation devices used in anterior cruciate ligament reconstruction. Orthop. Traumatol. Surg. Res.104, 203–207 (2018). CASGoogle Scholar
- Kundu, B., Rajkhowa, R., Kundu, S. C. & Wang, X. Silk fibroin biomaterials for tissue regenerations. Adv. Drug Del. Rev.65, 457–470 (2013). CASGoogle Scholar
- Yucel, T., Lovett, M. L. & Kaplan, D. L. Silk-based biomaterials for sustained drug delivery. J. Control. Release190, 381–397 (2014). CASGoogle Scholar
- Koh, L.-D. et al. Structures, mechanical properties and applications of silk fibroin materials. Prog. Polym. Sci.46, 86–110 (2015). CASGoogle Scholar
- Brown, J. E. et al. Injectable silk protein microparticle-based fillers: a novel material for potential use in glottic insufficiency. J. Voice33, 773–780 (2019). Google Scholar
- Marelli, B. et al. Programming function into mechanical forms by directed assembly of silk bulk materials. Proc. Natl Acad. Sci. USA114, 451–456 (2016). Google Scholar
- Li, C. et al. Regenerated silk materials for functionalized silk orthopedic devices by mimicking natural processing. Biomaterials110, 24–33 (2016). CASGoogle Scholar
- Guo, C. et al. Thermoplastic molding of regenerated silk. Preprint at ChemRxivhttps://doi.org/10.26434/chemrxiv.8343848 (2019).
- MedMarket Diligence. Global dynamics of surgical and interventional cardiovascular procedures, 2015–2022 (2016).
- Gori, T. et al. Predictors of stent thrombosis and their implications for clinical practice. Nat. Rev. Cardiol.16, 243–256 (2019). Google Scholar
- Finn, A. V. et al. Pathological correlates of late drug-eluting stent thrombosis: strut coverage as a marker of endothelialization. Circulation115, 2435–2441 (2007). Google Scholar
- Serruys, P. W., Garcia-Garcia, H. M. & Onuma, Y. From metallic cages to transient bioresorbable scaffolds: change in paradigm of coronary revascularization in the upcoming decade? Eur. Heart J.33, 16–25 (2011). Google Scholar
- Joner, M. et al. Pathology of drug-eluting stents in humans: delayed healing and late thrombotic risk. J. Am. Coll. Cardiol.48, 193–202 (2006). Google Scholar
- Jinnouchi, H. et al. Fully bioresorbable vascular scaffolds: lessons learned and future directions. Nat. Rev. Cardiol.16, 286–304 (2018). Google Scholar
- Wang, P.-J., Ferralis, N., Conway, C., Grossman, J. C. & Edelman, E. R. Strain-induced accelerated asymmetric spatial degradation of polymeric vascular scaffolds. Proc. Natl Acad. Sci. USA115, 2640–2645 (2018). CASGoogle Scholar
- Sharma, U. et al. The development of bioresorbable composite polymeric implants with high mechanical strength. Nat. Mater.17, 96–103 (2017). Google Scholar
- Kang, S. K. et al. Bioresorbable silicon electronic sensors for the brain. Nature530, 71–76 (2016). CASGoogle Scholar
- Boutry, C. M. et al. A sensitive and biodegradable pressure sensor array for cardiovascular monitoring. Adv. Mater.27, 6954–6961 (2015). CASGoogle Scholar
- Yu, K. J. et al. Bioresorbable silicon electronics for transient spatiotemporal mapping of electrical activity from the cerebral cortex. Nat. Mater.15, 782–791 (2016). CASGoogle Scholar
- Hwang, S. W. et al. A physically transient form of silicon electronics. Science337, 1640–1644 (2012). CASGoogle Scholar
- Tao, H. et al. Silk-based resorbable electronic devices for remotely controlled therapy and in vivo infection abatement. Proc. Natl Acad. Sci. USA111, 17385–17389 (2014). CASGoogle Scholar
- Tibbitt, M. W., Rodell, C. B., Burdick, J. A. & Anseth, K. S. Progress in material design for biomedical applications. Proc. Natl Acad. Sci. USA112, 14444–14451 (2015). CASGoogle Scholar
- Kang, S. K. et al. Dissolution chemistry and biocompatibility of silicon- and germanium-based semiconductors for transient electronics. ACS Appl. Mater. Interfaces7, 9297–9305 (2015). CASGoogle Scholar
- Kim, D.-H. et al. Dissolvable films of silk fibroin for ultrathin conformal bio-integrated electronics. Nat. Mater.9, 511–517 (2010). CASGoogle Scholar
- Hwang, S. W. et al. Materials for bioresorbable radio frequency electronics. Adv. Mater.25, 3526–3531 (2013). CASGoogle Scholar
- Lei, T. et al. Biocompatible and totally disintegrable semiconducting polymer for ultrathin and ultralightweight transient electronics. Proc. Natl Acad. Sci. USA114, 5107–5112 (2017). CASGoogle Scholar
- Huang, X. et al. Biodegradable materials for multilayer transient printed circuit boards. Adv. Mater.26, 7371–7377 (2014). CASGoogle Scholar
- Shou, W. et al. Low-cost manufacturing of bioresorbable conductors by evaporation-condensation-mediated laser printing and sintering of Zn nanoparticles. Adv. Mater.29, 1700172 (2017). Google Scholar
- Acar, H. et al. Study of physically transient insulating materials as a potential platform for transient electronics and bioelectronics. Adv. Funct. Mater.24, 4135–4143 (2014). CASGoogle Scholar
- Jamshidi, R., Çinar, S., Chen, Y., Hashemi, N. & Montazami, R. Transient bioelectronics: Electronic properties of silver microparticle-based circuits on polymeric substrates subjected to mechanical load. J. Polym. Sci. B Polym. Phys.53, 1603–1610 (2015). CASGoogle Scholar
- Boutry, C. M. et al. A stretchable and biodegradable strain and pressure sensor for orthopaedic application. Nat. Electron.1, 314–321 (2018). Google Scholar
- Hwang, S.-W. et al. High-performance biodegradable/transient electronics on biodegradable polymers. Adv. Mater.26, 3905–3911 (2014). CASGoogle Scholar
- Bettinger, C. J. & Bao, Z. Organic thin-film transistors fabricated on resorbable biomaterial substrates. Adv. Mater.22, 651–655 (2010). CASGoogle Scholar
- Chang, J. K. et al. Biodegradable electronic systems in 3d, heterogeneously integrated formats. Adv. Mater.30, 1704955 (2018). Google Scholar
- Hwang, S. W. et al. 25th anniversary article: materials for high-performance biodegradable semiconductor devices. Adv. Mater.26, 1992–2000 (2014). CASGoogle Scholar
- Yin, L. et al. Mechanisms for hydrolysis of silicon nanomembranes as used in bioresorbable electronics. Adv. Mater.27, 1857–1864 (2015). CASGoogle Scholar
- Lee, Y. K. et al. Dissolution of monocrystalline silicon nanomembranes and their use as encapsulation layers and electrical interfaces in water-soluble electronics. ACS Nano11, 12562–12572 (2017). CASGoogle Scholar
- Kang, S. K., Koo, J., Lee, Y. K. & Rogers, J. A. Advanced materials and devices for bioresorbable electronics. Acc. Chem. Res.51, 988–998 (2018). CASGoogle Scholar
- Oldreive, S. Safe intakes of vitamins and minerals: recommendations from the Expert Group on Vitamins and Minerals. Nutr. Bull.28, 199–202 (2003). Google Scholar
- Song, G. & Song, S. A possible biodegradable magnesium implant material. Adv. Eng. Mater.9, 298–302 (2007). CASGoogle Scholar
- Koo, J. et al. Wireless bioresorbable electronic system enables sustained nonpharmacological neuroregenerative therapy. Nat. Med.24, 1830–1836 (2018). CASGoogle Scholar
- Shin, J. et al. Bioresorbable pressure sensors protected with thermally grown silicon dioxide for the monitoring of chronic diseases and healing processes. Nat. Biomed. Eng.3, 37–46 (2019). CASGoogle Scholar
- Vert, M. et al. Terminology for biorelated polymers and applications (IUPAC Recommendations 2012). Pure Appl. Chem.84, 377–410 (2012). CASGoogle Scholar
- Villa, T. & Brianza, S. in Bioresorbable Polymers for Biomedical Applications: From Fundamentals to Translational Medicine (eds Perale, G. & Hilborn, J.) 95–100 (Woodhead, 2017).
- Ozdil, D., Wimpenny, I., Aydin, H. M. & Yang, Y. in Science and Principles of Biodegradable and Bioresorbable Medical Polymers (ed. Zhang, X.) 379–414 (Woodhead, 2017).
- U.S. Food and Drug Administration. Use of International Standard ISO 10993-1, “Biological evaluation of medical devices - Part 1: Evaluation and testing within a risk management process” (FDA, 2016).
- Guan, A. et al. Medical devices on chips. Nat. Biomed. Eng.1, 0045 (2017). CASGoogle Scholar
- Jannasch, M. et al. An in vitro model mimics the contact of biomaterials to blood components and the reaction of surrounding soft tissue. Acta Biomater.89, 227–241 (2019). CASGoogle Scholar
- Jannasch, M. et al. A comparative multi-parametric in vitro model identifies the power of test conditions to predict the fibrotic tendency of a biomaterial. Sci. Rep.7, 1689 (2017). Google Scholar
- Sharifi, F. et al. A foreign body response-on-a-chip platform. Adv. Healthc. Mater.8, 1801425 (2019). Google Scholar
- Kajahn, J. et al. Artificial extracellular matrices composed of collagen I and high sulfated hyaluronan modulate monocyte to macrophage differentiation under conditions of sterile inflammation. Biomatter2, 226–273 (2012). Google Scholar
- Kou, P. M. et al. Predicting biomaterial property-dendritic cell phenotype relationships from the multivariate analysis of responses to polymethacrylates. Biomaterials33, 1699–1713 (2012). CASGoogle Scholar
- McWhorter, F. Y., Wang, T., Nguyen, P., Chung, T. & Liu, W. F. Modulation of macrophage phenotype by cell shape. Proc. Natl Acad. Sci. USA110, 17253–17258 (2013). CASGoogle Scholar
- Nakamura, K. et al. High, but not low, molecular weight hyaluronan prevents T-cell-mediated liver injury by reducing proinflammatory cytokines in mice. J. Gastroenterol.39, 346–354 (2004). CASGoogle Scholar
- Sridharan, R., Cameron, A. R., Kelly, D. J., Kearney, C. J. & O’Brien, F. J. Biomaterial based modulation of macrophage polarization: a review and suggested design principles. Mater. Today18, 313–325 (2015). CASGoogle Scholar
- Chen, S. et al. Characterization of topographical effects on macrophage behavior in a foreign body response model. Biomaterials31, 3479–3491 (2010). CASGoogle Scholar
- Kamolratanakul, P. et al. Nanogel-based scaffold delivery of prostaglandin E2 receptor–specific agonist in combination with a low dose of growth factor heals critical-size bone defects in mice. Arthritis Rheum.63, 1021–1033 (2011). CASGoogle Scholar
- Lau, T. T. & Wang, D.-A. Stromal cell-derived factor-1 (SDF-1): homing factor for engineered regenerative medicine. Expert. Opin. Biol. Ther.11, 189–197 (2011). CASGoogle Scholar
- Shen, W. et al. The effect of incorporation of exogenous stromal cell-derived factor-1 alpha within a knitted silk-collagen sponge scaffold on tendon regeneration. Biomaterials31, 7239–7249 (2010). CASGoogle Scholar
- Kim, D.-H. & Martin, D. C. Sustained release of dexamethasone from hydrophilic matrices using PLGA nanoparticles for neural drug delivery. Biomaterials27, 3031–3037 (2006). CASGoogle Scholar
- Mercanzini, A. et al. Controlled release nanoparticle-embedded coatings reduce the tissue reaction to neuroprostheses. J. Control. Release145, 196–202 (2010). CASGoogle Scholar
- Chen, W. C. W. et al. Controlled dual delivery of fibroblast growth factor-2 and Interleukin-10 by heparin-based coacervate synergistically enhances ischemic heart repair. Biomaterials72, 138–151 (2015). CASGoogle Scholar
- Mokarram, N., Merchant, A., Mukhatyar, V., Patel, G. & Bellamkonda, R. V. Effect of modulating macrophage phenotype on peripheral nerve repair. Biomaterials33, 8793–8801 (2012). CASGoogle Scholar
- Son, D. et al. Bioresorbable electronic stent integrated with therapeutic nanoparticles for endovascular diseases. ACS Nano9, 5937–5946 (2015). CASGoogle Scholar
- Williams, D. F. The Williams Dictionary of Biomaterials (Liverpool Univ. Press, 1999).
- ASTM International. Standard guide for assessment of absorbable polymeric implants (ASTM, 2016).
- Wegst, U. G. K., Bai, H., Saiz, E., Tomsia, A. P. & Ritchie, R. O. Bioinspired structural materials. Nat. Mater.14, 23–26 (2015). CASGoogle Scholar
- Drogset, J. O., Straume, L. G., Bjørkmo, I. & Myhr, G. A prospective randomized study of ACL-reconstructions using bone-patellar tendon-bone grafts fixed with bioabsorbable or metal interference screws. Knee Surg. Sports Traumatol. Arthrosc.19, 753–759 (2011). Google Scholar
- Oiwa, H., Ishida, R. & Sudo, K. Sternal closure with reabsorbable pin and cord in pediatric less invasive cardiac surgery. Ann. Thorac. Surg.78, 358–359 (2004). Google Scholar
- Saito, T., Iguchi, A., Sakurai, M. & Tabayashi, K. Biomechanical study of a poly-L-lactide (PLLA) sternal pin in sternal closure after cardiothoracic surgery. Ann. Thorac. Surg.77, 684–687 (2004). Google Scholar
- Tatsumi, A., Kanemitsu, N., Nakamura, T. & Shimizu, Y. Bioabsorbable poly-L-lactide costal coaptation pins and their clinical application in thoracotomy. Ann. Thorac. Surg.67, 765–768 (1999). CASGoogle Scholar
- Jarvela, T. et al. Double-bundle anterior cruciate ligament reconstruction using hamstring autografts and bioabsorbable interference screw fixation: prospective, randomized, clinical study with 2-year results. Am. J. Sports Med.36, 290–297 (2008). Google Scholar
- Eppley, B. L. & Reilly, M. Degradation characteristics of PLLA-PGA bone fixation devices. J. Craniofac. Surg.8, 116–120 (1997). CASGoogle Scholar
- Goldstein, J. A., Quereshy, F. A. & Cohen, A. R. Early experience with biodegradable fixation for congenital pediatric craniofacial surgery. J. Craniofac. Surg.8, 110–115 (1997). CASGoogle Scholar
- Pietrzak, W. S. & Eppley, B. L. Stability of craniofacial PLLA/PGA copolymer bioabsorbable screws. J. Craniofac. Surg.17, 331–336 (2006). Google Scholar
- Bowen, P. K., Drelich, A., Drelich, J. & Goldman, J. Rates of in vivo (arterial) and in vitro biocorrosion for pure magnesium. J. Biomed. Mater. Res. A103, 341–349 (2015). Google Scholar
- Nie, F. L., Zheng, Y. F., Wei, S. C., Hu, C. & Yang, G. In vitro corrosion, cytotoxicity and hemocompatibility of bulk nanocrystalline pure iron. Biomed. Mater.5, 065015 (2010). CASGoogle Scholar
- Wang, H. & Shi, Z. In vitro biodegradation behavior of magnesium and magnesium alloy. J. Biomed. Mater. Res. B Appl. Biomater.98, 203–209 (2011). Google Scholar
- Fellman, M. Researchers demonstrate first example of a bioresorbable electronic medicine. McCormick School Engineer. Northwestern Univ.https://www.mccormick.northwestern.edu/news/articles/2018/10/researchers-demonstrate-first-example-of-a-bioresorbable-electronic-medicine.html (2018).
- Kerecman Myers, D. et al. From in vivo to in vitro: the medical device testing paradigm shift. ALTEX34, 479–500 (2017). Google Scholar
Acknowledgements
We thank the NIH (R01AR068048, 5P41EB002520) and Stepping Strong Foundation, Brigham and Women's Hospital (A.N.) for support of this work. We also thank our many past students who have contributed to some of the foundations discussed here, as well as our many collaborators over the years.